Respiratory Muscle Training using a resistive load device improves quality of life in patients with COPD more effectively than threshold load devices
In a threshold RMT device, no significant flow is is achieved below the threshold; once the threshold pressure is overcome, a valve opens and the inspiratory flow is unrestricted. The threshold pressure is normally exceeded within the first 20% of inspiratory volume (Fig.1 [1]). This results in a breathing pattern with a sharp and brief pressure peak followed by a neutral phase with low effort (Fig. 2 [1]).
Resistive RMT devices force the inspiratory flow through an adjustable orifice. The applied pressure to achieve inspiratory flow therefore has to be maintained throughout the whole breath, utilizing the entire inspiratory volume for mus-
cle training (Fig.1 [1]). The associated breathing pattern shows limited, but more sustained pressure efforts (Fig. 2 [1]). Certain devices, such as the Breather, apply the same principle to the expiratory flow, targeting RMT to both inspiratory and expiratory muscles.
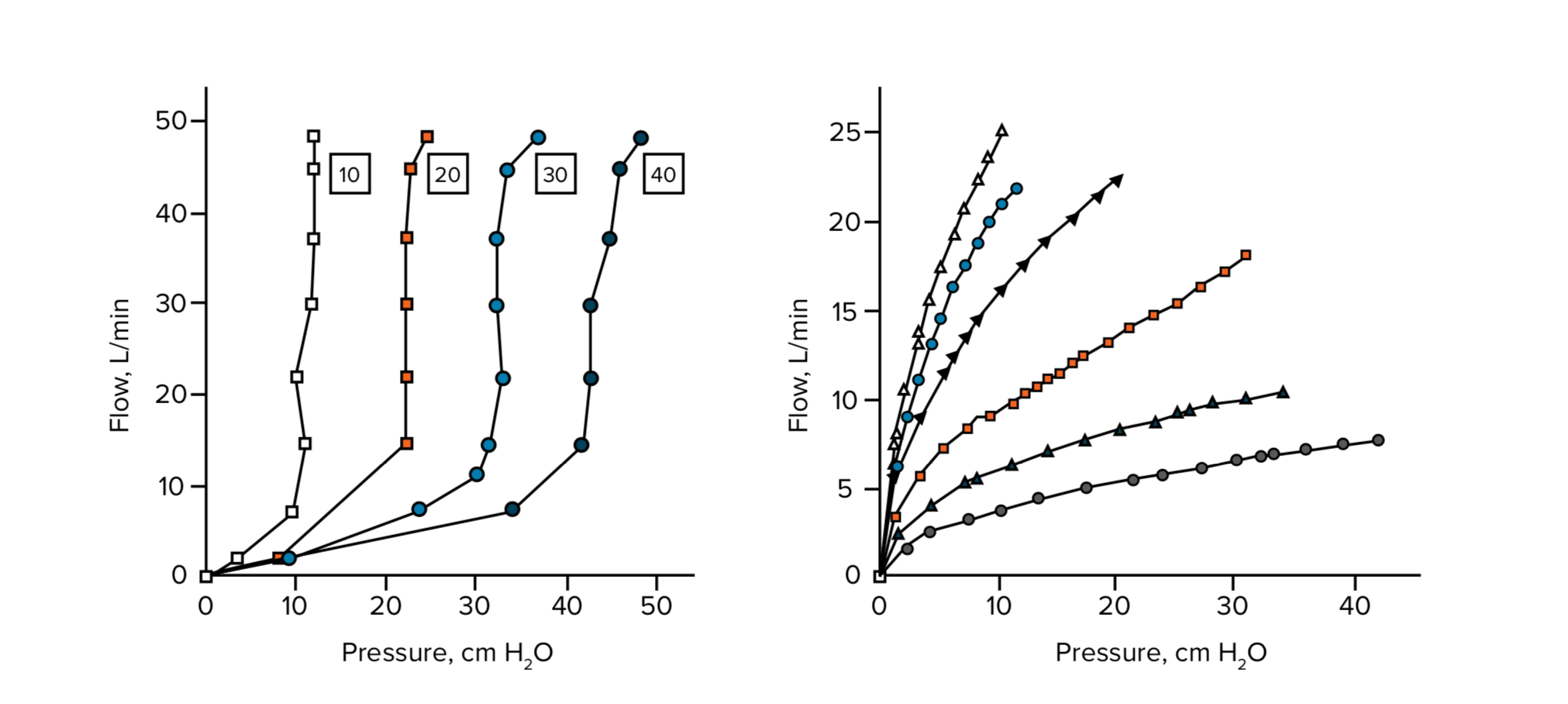
Figure 1: Inspiratory pressure plotted against flow rate in a threshold device (left) and a resistive device (right) [1].
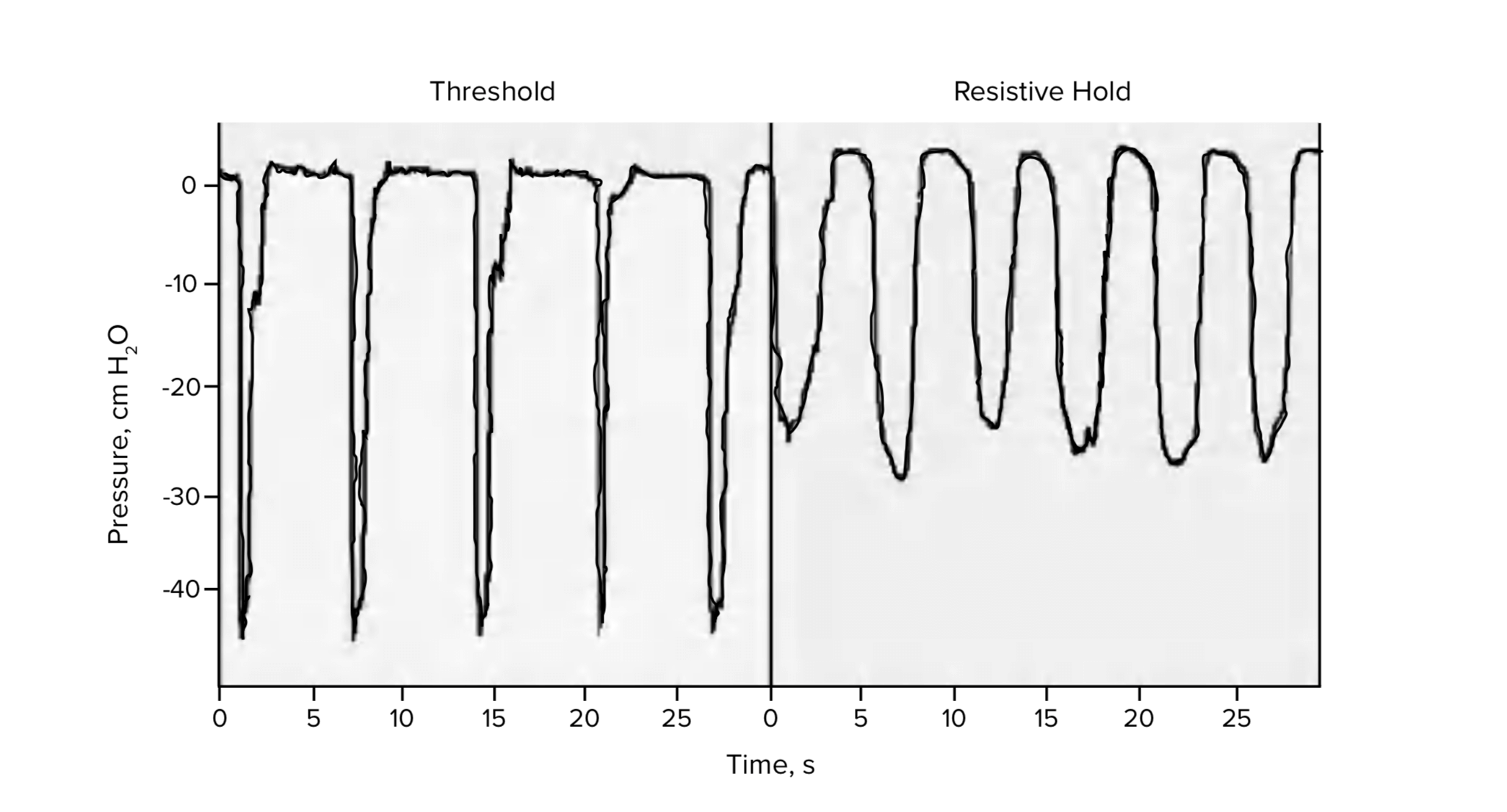
Figure 2: Representative examples to demonstrate differences in breathing patterns using a threshold (left) or resistive (right) device [1].
Three independent research publications have directly compared the efficacy of threshold and resis- tive RMT in a total of 124 patients with moderate to severe COPD. The studies concluded that both methods were effective in strengthening respiratory musculature and alleviating symptoms of COPD.
Hsiao FS et al assessed pulmonary function, inspiratory muscle strength and endurance, exercise ca- pacity, dyspnea and health-related quality of life (hrQOL) in COPD patients before and after 8 weeks of RMT with either a threshold or resistive inspiratory muscle training (IMT) device. Both muscle strength and exercise capacity increased due to either method of RMT training, as measured by maximal inspi- ratory pressure (MIP) and 6-minute walk test (6MWT), respectively. Respiratory muscle endurance time (RMET) improved significantly after either threshold or resistive RMT. Therefore, both methods lead to clinically relevant improvements of respiratory function in COPD patients, which was reflected in in- creased exercise capacity. Patients comments appreciated the cost effectiveness of the resistive RMT device [2].
Madariaga et al measured pulmonary function, oxygen uptake and hrQOL in COPD patients before and after 6 weeks of training using either a threshold or a resistive RMT device. Both training devices re- sulted in improvement in respiratory muscle function and overall hrQOL when compared to the control group. Specifically, both threshold and resistive RMT significantly improved MIP and esophageal pres- sure, and the threshold method also resulted in a significant increase in endurance time at 66% of the maximum load. Among the two training groups, only patients using the resistive RMT device reported significant improvements in all four aspects of health-related quality of life – dyspnea, fatigue, emotional function and mastery of the disease. This comparative evaluation of threshold and resistive RMT devic- es therefore demonstrates the equality of both methods in improving overall respiratory function and health status in COPD patients, as well as a noticeably higher efficacy of resistive RMT in improving all aspects of hrQOL [1].
Wu et al. compared COPD patients using a resistive IMT (R-IMT) device to a group using a threshold IMT (T-IMT) device and to a control group not doing RMT. The study period was 8 weeks, and RMT was performed 15 min twice a day each day with an intensity of 60% of MIP. They compared MIP, hrQOL, dyspnea, and maximal exercise capacity (using an ergometer; including endurance exercise capacity, maximum work (Wmax), peak oxygen uptake (VO2max), and carbon dioxide equivalent (VE/VCO2)). Both RMT groups showed significant and comparable improvement of MIP, dyspnea and QOL when compared to the control group. R-IMT was significantly superior to T-IMT with regards to all aspects
of hrQOL and exercise capacity. Here, R-IMT significantly improved VO2max compared to the control group, whereas the improvement gained by T-IMT failed to reach significance compared to the control group. R-IMT was superior to T-IMT in improving endurance exercise capacity, Wmax and VE/VCO2). Wu et al conclude that the effect of RMT using a resistive device was found to be superior to RMT us- ing a threshold device in this patient group [3].
In summary, three studies comparing the effects of threshold and resistive RMT on respiratory function, exercise capacity and hrQOL in COPD patients demonstrate clinically relevant efficacy of both methods in improving different respiratory and health status related parameters. In addition, resistive RMT has proven superior to threshold RMT with regards to hrQOL, exercise capacity and endurance, including VO2max.
REFERENCES
- Madariaga VB, Gáldiz Iturri JB, Manterola AG, Buey JC, Sebastián NT, Peña VS. Comparison of 2 Methods for Inspiratory Muscle Training in Patients With Chronic Obstructive Pulmonary Disease. Arch Bronconeu- mol. 2007;43: 431–8431.
- Hsiao SF, Wu YT, Wu HD, Wang TG. Comparison of effectiveness of pressure threshold and targeted re- sistance devices for inspiratory muscle training in patients with chronic obstructive pulmonary disease. J Formos Med Assoc. 2003;102: 240–245.
- Wu W, Guan L, Zhang X, Li X, Yang Y, Guo B, et al. Effects of two types of equal-intensity inspiratory muscle training in stable patients with chronic obstructive pulmonary disease: A randomised controlled trial. Respir Med. 2017;132: 84–91.
0 Comments